Tuhina Srivastava
Neighborhood Vulnerability and COVID-19 Vaccination Coverage in Philadelphia, PA
Abstract
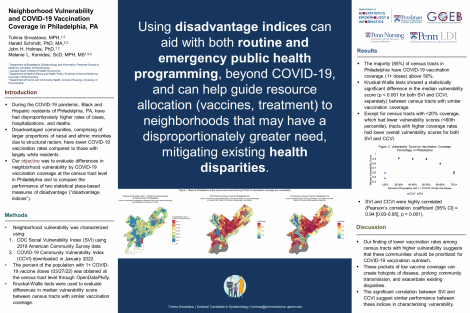
During the COVID-19 pandemic, residents of color living in disadvantaged communities in Philadelphia, Pennsylvania had disproportionately higher rates of cases, hospitalizations, and deaths, as well as lower rates of COVID-19 vaccination compared to largely white communities. Given these disparities, our objective was to evaluate differences in neighborhood vulnerability by COVID-19 vaccination coverage at the census tract level in Philadelphia and to compare the performance of two statistical place-based measures of disadvantage (“disadvantage indices”). Neighborhood vulnerability was characterized by the CDC Social Vulnerability Index (SVI) and COVID-19 Community Vulnerability Index (CCVI). COVID-19 vaccination coverage (percent of population with 1+ vaccine doses) was obtained at the census tract level through OpenDataPhilly. Kruskal-Wallis tests showed a statistically significant difference in the median vulnerability score (p>0.001 for both SVI and CCVI, separately) between census tracts with similar vaccination coverage. Except for census tracts with <20% coverage, which had lower vulnerability scores (<60th percentile), tracts with higher coverage rates had lower overall vulnerability scores for both SVI and CCVI. SVI and CCVI were also highly correlated (Pearson correlation coefficient [95% CI] = 0.94 [0.93-0.95], p<0.001), suggesting similar performance between these indices in characterizing vulnerability. Our finding of lower vaccination rates among census tracts with higher vulnerability suggests that these communities should be prioritized for COVID-19 vaccination outreach. Using disadvantage indices can aid with both routine and emergency public health programming, beyond COVID-19, and can help guide resource allocation to neighborhoods that may have a disproportionately greater need, mitigating existing health disparities.
Keywords
vaccination, COVID-19, health disparities, disadvantage, vulnerability, vaccines, neighborhoodAbout Us
To understand health and disease today, we need new thinking and novel science —the kind we create when multiple disciplines work together from the ground up. That is why this department has put forward a bold vision in population-health science: a single academic home for biostatistics, epidemiology and informatics.
© 2023 Trustees of the University of Pennsylvania. All rights reserved.. | Disclaimer



Comments